By Yunru Huang, Stella Aslibekyan, and Robert Gentleman*
Parenthood has its rewards, but a good night’s sleep isn’t one of them.
According to a National Sleep Foundation (NSF) poll, 38 percent of parents reported less than the recommended 7 hours of sleep per night. Some even lost almost 200 hours of sleep per year due to their children’s nighttime awakenings. Scientists examining sleep data from 23andMe research participants tested the hypothesis that parents, particularly single ones, sacrifice both sleep quality and duration for their offspring.

Measuring Sleep Quality
At the end of 2017, 23andMe launched the validated Pittsburgh Sleep Quality Index (PSQI) survey to study people’s sleep habits. The PSQI global score (0-21, higher is worse) is created by summing values on 7 subscores (each ranging from 0 to 3) representing different sleep aspects over the past month.
A PSQI score above 5 indicates poor/bad overall sleep quality, and sleep duration of less than 7 hours per 24-hour period means insufficient sleep.
Parenthood
To ascertain our participants’ parenthood status, we asked, “How many children under 6 live in your house?” and “How many biological children do you have?” Our parent sample was restricted to participants who reported having at least one child under 6 in the house and/or one biological child. We additionally restricted our sample to people between 20 and 50, a generation of potential parents with young children. A total of 239,562 research participants with available sleep data were included in this study.
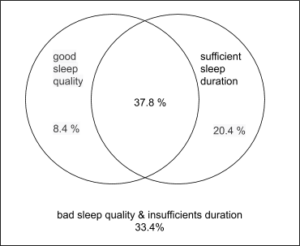
Figure 1. Proportions of sleep quality and duration in 23andMe participants who were 20 – 50 years old; PSQI score of 5 or less indicates good sleep quality; At least 7 hours per 24-hour period indicates sufficient sleep duration; N= 239,562; There are four groups in this plot: 1) good sleep quality & insufficient sleep duration: 8.4 percent 2) good sleep quality & sufficient sleep duration: 37.8 percent 3) bad sleep quality & sufficient sleep duration 20.4 percent 4) bad sleep quality & insufficient duration: 33.4 percent.
Approximately 42.2 percent of our participants reported sleeping less than 7 hours per night, and 53.8 percent experienced poor overall sleep quality assessed by PSQI.
Sufficient sleep duration also did not guarantee good sleep quality. Despite sleeping at least 7 hours a night, 20.4 percent of participants reported poor sleep quality. Moreover, 8.4 percent still reported sleeping well, albeit insufficiently long (Figure 1).
Moms and Dads and Sleep
Females had slightly longer self-reported sleep duration (Figure 2, right panel) and much worse overall sleep quality (Figure 2, left panel). Self-reported sleep duration decreased with age (Figure 2, right panel), although overall sleep quality became stable (Figure 2, left panel).
About half of our participants were parents. Perhaps unsurprisingly, we found that parents reported worse sleep.
For example, 47.2 percent of parents reported having insufficient sleep, compared to only 36.9 percent of non-parents. After adjusting for the effects of age and sex, parents were 45 percent more likely to report inadequate sleep (odds ratio (OR): 1.45, 95 percent confidence interval (CI): 1.42-1.48) and 3 percent more likely to report poor overall sleep quality (OR: 1.03, 95 percent CI: 1.01-1.05) compared to those without kids.
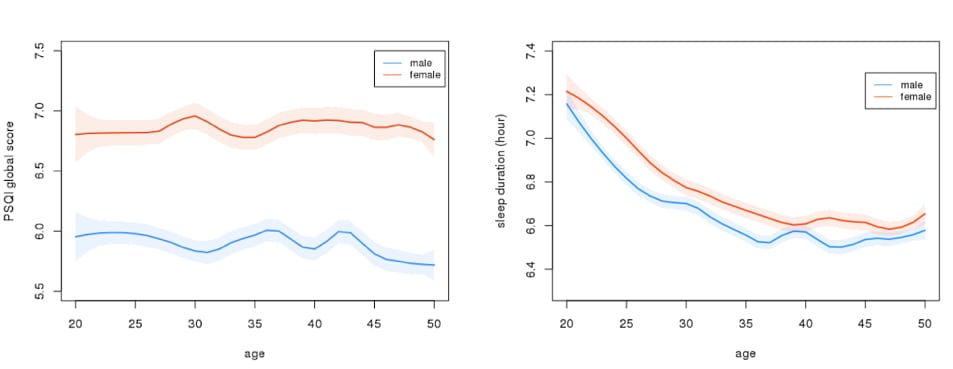
Figure 2. Sleep quality and duration by age (among 20 – 50 year olds) and sex in 23andMe participants. Sleep quality is measured by PSQI global scores (0-21), with higher scores indicating worse sleep; Sleep duration (0-16 hours) was self-reported per night. Due to computational limitations, we randomly selected 45,000 females and 45,000 males for these two plots.
Sleep and Marital Status
In addition to the PSQI sleep survey and questions about parenthood, we asked participants about their marital status. The possible responses were “now married,” “widowed,” “divorced,” “separated,” or “never married.” Almost 88.9 percent of our 239,562 study participants responded to this question.
Of the respondents, 40.2 percent were parents and answered “now married,” and we defined them as “married parents.” We classified 10.3 percent of respondents as “single parents;” they self-identified as “widowed,” “divorced,” “separated,” or “never married.” The rest were married couples (15.6 percent) or single people (33.8 percent) without children.
The prevalence of bad sleep was even higher among single parents. 53.7 percent of single parents and 45.1 percent of married parents reported insufficient sleep duration. (Figure 3, left panel). After adjusting for age and sex, single parents were 44 percent more likely to report inadequate sleep duration than their married counterparts (OR: 1.44, 95 percent CI: 1.40-1.48).
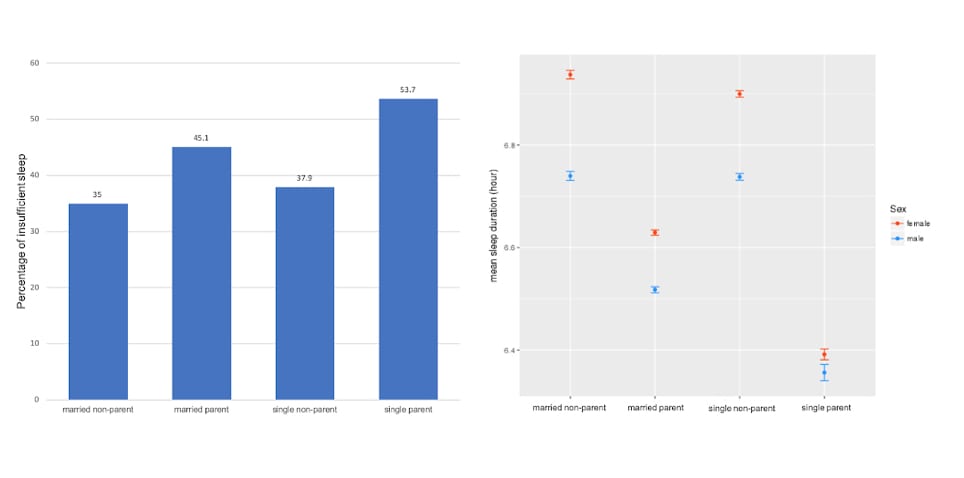
Figure 3. Relationships between sleep duration and parenthood in 23andMe participants who were 20-50 years of age. Sleep duration (0-16 hours) were self-reported duration per night, and less than 7 hours of sleep duration per 24-hour period indicates insufficient sleep; N: total: 212,923; married non-parent: 33,174, married parent: 85,754, single non-parent: 21,992, single parent: 72,003; female: 128,467, male: 84,456.
Sleep and the Single Parent
Similarly, 61.4 percent of single parents and 50.3 percent of married parents reported poor sleep quality (Figure 4, left panel).
After adjusting for age and sex, single parents were 50 percent more likely to report sleeping poorly (OR: 1.50, 95 percent CI: 1.46-1.54). The reasons for this discrepancy might go beyond sharing the workload of parenting; single parents may also miss out on the emotional support available in committed relationships. In other studies, being happily married was associated with better physical, mental, and emotional health—factors that might also improve sleep quality.
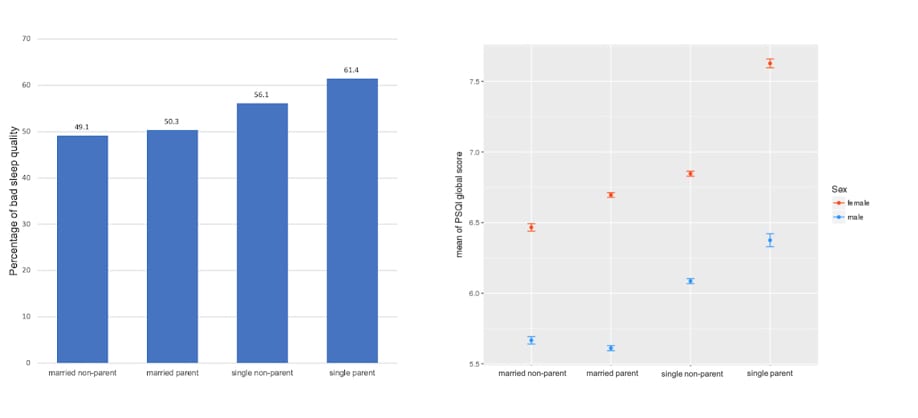
Figure 4. Relationships between sleep quality and parenthood in 23andMe participants who were 20-50 years of age. PSQI score of 5 or less indicates good sleep quality; N: total: 212,923; married non-parent: 33,174, married parent: 85,754, single non-parent: 21,992, single parent: 72,003; single_parent: 72,003; female: 128,467, male: 84,456.
We also observed that single moms had the worst sleep quality (Figure 4, right panel) across all groups. For the self-reported sleep duration, we found that single moms and dads were similar (OR: 0.95, 95 percent CI: 0.89-1.01), and had fewer sleep hours than other groups (Figure 3, right panel).
Other Factors Affecting Sleep
Sleep patterns are also affected by other influential factors.
For example, after adjusting for age, sex, and marital status, participants with depression were 31 percent more likely to report insufficient sleep duration (OR: 1.31, 95 percent CI: 1.29-1.33), and 184 percent more likely to have poor overall sleep quality (OR: 2.84, 95 percent CI: 2.79-2.90). People suffering from chronic pain also were 4.14 times more likely to report insufficient sleep per night (OR: 4.14, 95 percent CI: 3.96-4.33) and were 69 percent more likely to report poor overall sleep quality (OR: 1.69, 95 percent CI: 1.63-1.74).
Also, we observed that our PSQI sleep survey respondents** were more likely to be female (OR: 1.30, 95 percent CI: 1.29-1.31 ) and single (OR: 1.09, 95 percent CI: 1.08-1.10). We also invited our customers to answer another question to rate their sleep quality directly and found our PSQI sleep survey respondents were more likely to have good self-rated sleep quality (OR: 1.03, 95 percent CI: 1.02-1.03 ) compared to those who did not answer the survey.
In summary, we found that parenthood is associated with impairments in sleep quality and duration– particularly for single parents. To further advance our understanding of sleep, 23andMe is currently actively investigating associations between more than a thousand other lifestyle, clinical, and socioeconomic phenotypes and sleep quality. We would love for you to help us study sleep — if you are a research participant, you can find our latest sleep quality survey by searching for “Your Sleep Quality” while logged in.
*Yunru Huang is a scientist in Biostatistics at 23andMe. Robert Gentleman, Ph.D., is 23andMe’s vice president of computational biology, and Stella Aslibekyan is a Genetic Epidemiologist on our research team.
** For all 23andMe customers who consented to research, a person was deemed to be a “PSQI sleep survey respondent” if he/she completed the Pittsburgh Sleep Quality Index (PSQI) survey and a “PSQI sleep survey non-respondent” if he/she did not.