Editor’s note: We posted this a couple of years ago, but in light on the historic agreement between the family of Henrietta Lacks and National Institutes of Health, we thought it worthy of re-posting. Also read Carl Zimmer’s great piece in the New York Times. The post has been slightly changed from the original.
Henrietta Lacks was only 31 years old when she died on October 4, 1951. But thanks to one of the more shameful, yet at the same time scientifically beneficial, episodes in the history of medical science, cells from the tumor that killed her grow today in laboratories all over the world.
An Aggressive Cancer
Henrietta Lacks’ story is a powerful scientific and ethical lesson for researchers who work with human subjects. It all started in February 1951, when Dr. George Gey of Johns Hopkins was given a sample of cervical cancer cells that had been taken from a young African American woman who was dying of cervical cancer.
Gey wanted the cells because he was one of many scientists trying to find a way to grow human cells in for an extended period of time in the laboratory. It had been done with animal cells, but no one could get human cells to keep growing for more than a few weeks.
Ms. Lacks’ cells were different. Her tumor grew so aggressively that at her autopsy, just eight months after the cells were removed, it was found that her cancer had infiltrated her entire body.
HeLa Cells
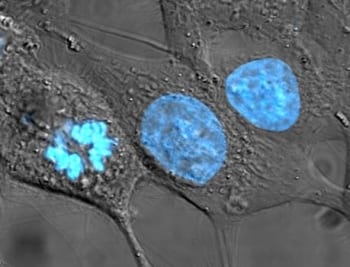
These extraordinary growth properties, while deadly for Henrietta, were probably what brought success to Gey. He was able to keep the cells growing in a dish long-term, and he soon found himself sending samples to other scientists who wanted to study human cells, who then passed them on to their colleagues, and so on and so on.
Soon HeLa cells, as they were called (Henrietta Lacks), were everywhere and being used for everything — cancer research, drug testing, even development of the polio vaccine. The lessons learned from growing these cells also allowed scientists to coax other cells to survive in the Petri dish, ushering in a new era of biology.
But as the number of cell lines scientists had established grew, a problem emerged. It can be very difficult to distinguish two different types of cells just by looking at them under a microscope. How could a researcher know for sure which kind of cells their colleagues had sent them? How could they check to make sure they hadn’t mixed them up?
G6PD
In the late 1960s, a scientist named Stan Gartler came up with a plan.
None of the DNA technologies so commonplace today, such as SNP chips, were around back then, but scientists did know about genetic variation between people. They had observed that for certain proteins, some people made one version, while other people made a different version.
One of the variable proteins Garlter focused on was an enzyme called glucose-6-phosphate dehydrogenase (G6PD) that helps to protect cells from damage. There are two forms — A and B. The A version is primarily found in people with African ancestry. People with other ethnic backgrounds almost never have this version.
It wasn’t known then, but the two different forms of G6PD are the result of a single SNP.
(In addition to the A and B forms, there are actually other forms of the G6PD gene that cause a person to completely lack the G6PD protein. Read more in the 23andMe Carrier Status Report for G6PD deficiency. 23andMe customers can figure out whether they have type A or type B G6PD using the table at the end of this post).
Unique Cell Lines
Gartler also looked at an enzyme called phosphoglucomutase (PGM) that comes in three forms: 1, 1-2, and 2.
And now it’s time to cue the dramatic music:
Gartler was given 18 supposedly unique human cell lines by the American Type Culture Collection, a repository that scientists could order different types of cells from. One of the 18 was a vial of HeLa cells. The rest were all different types of cells, many allegedly from Caucasian people.
When Gartler tested the G6PD and PGM proteins in these 18 cell lines, he got a surprising result. All of them had the G6PD type A and PGM type 1.
There was no way this could be right. The cells from Caucasians should not have been G6PD type A. And even if all the cells had come from African Americans, it was still too much of a coincidence. In his report of his findings published in Nature, Gartler calculated that the chance of all 18 cell lines being G6PD type A and PGM type 1 was “absurdly low” — 1 in 6,000,000,000,000,000.
HeLa Cells Around the World
Every single one of the cell lines Gartler was investigating, and countless others being used around the world, had been contaminated by HeLa cells. They had taken over every Petri dish of cells they had come near.
Gartler and others sounded the alarm to the scientific community, but many did not listen. Admitting that the cells they thought they had been working with were really HeLa cells was just too embarrassing and potentially devastating to so many careers. So people chose to just ignore the problem.
Unfortunately, HeLa cell contamination continues today. There are still cell banks selling HeLa cells under other names, often claiming that they are totally different types of cells. Scientists think they are getting a batch of oral cancer cells or liver cells, but in reality, it’s just another batch of HeLa cells.
A Lack of Informed Consent
Questions about the startling ubiquity of HeLa cells are not the only ones that have been raised since Henrietta Lacks’ death. It has become clear over the decades that by not asking her permission for her cells, or informing her family about how they were being used in experiments and bought and sold literally by the millions, scientists have dishonored a woman whose death has brought life to so many others.
The emotional impact of this saga on her family has been enormous. They knew nothing of HeLa cells until they were contacted several decades after Henrietta’s death. It was by scientists who were looking for blood samples that could help them tease out more information from the HeLa cells. Imagine the shock of being told that a lost loved one was alive, in a sense, in a freezer at a university.
The family, poor and undereducated, thought they were being tested to see if they would die of cancer too. When researchers never got back to them they were left to wonder about their own fates. Today they understand more about what has happened. However, that doesn’t change the fact that they feel betrayed.
The Immortal Life of Henrietta Lacks
The questions of who owns a tissue sample or has permission to use it is hotly debated. And what are the responsibilities of researchers especially when there is money involved? (For information on how 23andMe deals with these issues, please read our privacy statement, terms of service and consent form.) For more on this aspect of the Henrietta Lacks story, check out writer Rebecca Skloot’s website. There you’ll find excerpts of her book on the subject, “The Immortal Life of Henrietta Lacks.” (The book was published in 2010 and became a bestseller.)
The G6PD gene is on the X chromosome. That means that men have one copy and women have two. Men will therefore either be type A or B. Women on the other hand can have both types of the enzyme. The type of G6PD enzyme expressed in each of a woman’s cells depends on which of her X chromosomes is “inactivated”. 23andMe customers can check their data at rs1050829 to figure out their G6PD type.
| Genotype | G6PD Type | |
|---|---|---|
| Men | ||
| C | A | |
| T | B | |
| Women | ||
| CC | A | |
| TT | B | |
| CT | A/B |