This week, 23andMe and 20 nonprofits, advocacy groups, and research institutions launched a new Lung Cancer Genetics Study. This study unites patients, advocates, doctors, and scientists to transform our understanding of the genetics of lung cancer with the hope of advancing research toward finding a cure.
Through this collaborative study, we aim to recruit 10,000 people diagnosed with lung cancer to participate in this crucial research that could help others in the future.
A Broad Collaboration
Those who participate will help 23andMe and collaborating organizations create a repository of genetic and other data for lung cancer research by qualified scientists. This research data could be used to better identify those at the highest risk for lung cancer and discern how genetic and lifestyle factors play a role. The study could also improve earlier detection through enhanced screening. In addition, the research could also be used to develop more personalized treatments, as genetic research can help inform more targeted therapies.
Together, we’ll learn more about the genetic factors that impact lung cancer and better identify those at the most significant risk. Ultimately, we want to advance research towards finding a cure.
“The link between genetics and lung cancer can transform our understanding of risk and treatment,” said Jill Feldman, a co-founder of the patient advocacy group EGFR Resisters, a community of people diagnosed with and/or personally affected by EGFR-positive lung cancer.
Jill said seeing such a broad collaboration of groups supporting this study is heartening.
“For the first time, the entire lung cancer community—patients, advocates, doctors, researchers—unites to support this vital study,” said Jill.
Todd Fielder, who is active with the patient advocacy group RET Positive and is a stage 4 lung cancer patient, said the broad coalition supporting this study is motivating.
“I want to participate in research to help move science forward, to hopefully come up with new treatment options,” said Todd. “If not for myself, then for future generations.”
About Lung Cancer
Lung cancer is the number one cause of cancer deaths in both men and women in the United States. In 2020, more people died from lung cancer than breast, colorectal, and prostate cancer combined, according to the American Cancer Society Cancer Facts & Figures 2023 report. About one in 16 men and one in 17 women in the United States will be diagnosed with lung cancer in their lifetime, the report indicates. It is the third most common form of cancer in the United States, according to the Centers for Disease Control (CDC). Despite being the deadliest cancer, lung cancer research is underfunded compared to other cancer types. Lung cancer receives $10,000 per death in federal and non-profit cancer funding, whereas breast cancer receives $91,000 per death.
Lung cancer usually begins in the lungs as either a small cell or non-small cell cancer. These two forms grow differently and are treated differently. Although it first starts in the lungs, the cancer may spread to lymph nodes or other areas of the body, such as the brain. When a cancer spreads from one part of the body to another, it’s called metastasis.
While most of us know that smoking increases one’s risk, between 10–20 percent of people who develop lung cancers have never smoked or smoked less than 100 cigarettes in their lifetime. Two-thirds of these people are women. Researchers at Harvard made an interesting finding among lung cancer patients who never smoked. Still, they had a family history of lung cancer, pointing to a specific genetic mutation in the epidermal growth factor receptor gene, EGFR. Published in the scientific journal Nature Genetics, the study found that an EGFR mutation that is present in many patients’ tumors increases the risk of developing lung cancer when it is inherited genetically. It has been estimated that this EGFR T790M mutation is a major cancer predisposition gene, with carriers having an estimated 31% risk of developing lung cancer.
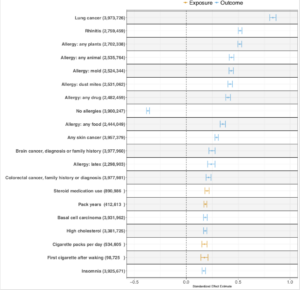
In fact, there are many factors, both genetic and non-genetic, that can contribute to lung cancer risk that are not related to smoking. Environmental exposures, other health conditions, lifestyle, and genetics can all play a role. Internal 23andMe data found that a family history of lung cancer, along with different types of allergies or rhinitis, the stuffed or dripping nose caused by allergies, were all associated with lung cancer, but that association does not mean that they were causal.
Environmental Factors in Lung Cancer Risk
Air pollution also contributes to the development of lung cancer. One study published in the academic journal Nature found that higher rates of air pollution known as PM2.5 are associated with higher rates of lung cancer with mutations in the EGFR gene. The researchers also showed that air pollution may contribute to lung cancer development by helping push lung cells with cancer-causing EGFR mutations over the edge from precancerous to cancerous. Cases of lung cancer are unevenly distributed throughout the United States, with much of the difference between states attributed to factors such as tobacco addiction. Interestingly, however, many areas with higher lung cancer rates also have high levels of PM2.5 air pollution, underscoring the complex relationship between our health and lifestyle factors, socioeconomic factors, and environmental exposures.
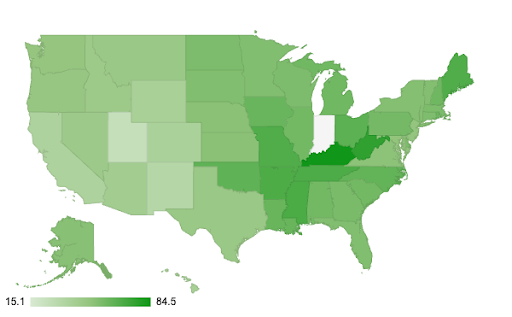
State by State Cancer rate per 100,000 people. Source: U.S. Cancer Statistics Working Group. https://www.cdc.gov/cancer/dataviz, released in June 2024.
While the genetics of lung cancer are not yet well understood, it’s estimated that up to 15% of people diagnosed with lung cancer may have DNA variants linked to cancer development. One study of 5000 people diagnosed with lung cancer in Utah found that those with a family history of lung cancer in their immediate family (like parents, siblings, or children) were more than twice as likely to be diagnosed with lung cancer as people with no family history. The risk generally increased with the number of diagnosed family members. Even individuals with only second or third-degree relatives affected by lung cancer were at higher risk. (Second-degree relatives include family members like grandparents, aunts, uncles, nieces, nephews, and half-siblings; third-degree relatives include family members like great-grandparents, great-aunts, great-uncles, and first cousins.)
Understanding more about the role that both the environment and genetics play in lung cancer will help scientists work to develop new and more personalized therapies. This is particularly true for people who develop lung cancer at an early age or who don’t have known risk factors such as smoking history or radon exposure, which is another known cause of lung cancer.
More about the Lung Cancer Genetics Study
Like all 23andMe research, a research ethics committee will oversee the Lung Cancer Genetics Study. In the United States, this is called an Institutional Review Board (IRB), which is an independent ethics panel that ensures research is conducted in accordance with government and ethical guidelines.
23andMe’s unique research platform — its ability to enroll participants online — makes it ideal for this study. The de-identified data from this study will be made available to approved researchers and to approved nonprofit researchers and institutions at no cost. Along with de-identified genetic data, the scientific database will include data from surveys on participants’ lung cancer experience and, in some cases, data from medical records and tumor testing.
The Lung Cancer Genetics Study is made possible by Troper Wojcicki Philanthropies.
To learn more about the study, our collaborators, and eligibility criteria, visit the Lung Cancer Genetics Study landing page.




