By Daniella Coker, MPH, and Janie Shelton, Ph.D.*
Several studies show the three COVID-19 vaccines being used in the United States — from Johnson & Johnson (J&J), Moderna, and Pfizer — are safe1,2 and effective2,3 and offer the best hope to beat the pandemic.2,4 And as so many of us have gotten vaccinated, it’s impossible not to notice that people react differently to the vaccines. Many people report having no reaction, while others feel sick enough to stay home in bed. 23andMe researchers wanted to know more about why. Is it due to the type of vaccine, our age, or something else?
To learn more about these differences we analyzed the data from more than 100,000 23andMe consented research participants and found that the second in the two-shot vaccine from Moderna produced the strongest reactions. We also learned that younger people and women tended to react more to the vaccine than others.
Get Vaccinated
But before going into what our researchers found, we should be clear: The side effects of vaccines are minimal, while the risks from the virus caused by COVID-19 are severe. This was further confirmed by new data from the CDC. More than 35 million people in the United States have contracted the virus caused by COVID-19, and 614,000 of them have died. Even with the emerging Delta variant cases, the most significant risk is remaining unvaccinated. We encourage people to take the advice of healthcare professionals, the World Health Organization, state and local public health officials, and the CDC and get vaccinated.
23andMe’s researchers wanted to examine differences in how sick people felt after receiving the vaccines. Now that more than half the U.S. population has been fully vaccinated and about 60 percent have had at least one shot,5 our scientists wanted to explore how people react differently to different vaccines and what factors may influence those differences. This study does not look at adverse reactions but categorizes how people felt after they were vaccinated and compares the degree of “feeling sick” between three different vaccines.
For 23andMe’s study, consented research participants were asked three questions: (1) What was their most recent COVID-19 vaccination? (2) What symptoms, if any, did they experience? and (3) How sick did they feel afterward.
Most research participants reported that their most recent vaccination was their second dose of either the Pfizer (44%) or Moderna (38%) vaccine.

Approximately half of respondents didn’t feel sick, 40% felt a little or somewhat ill, and 10% felt very or extremely sick. And to be clear, “feeling sick” as a reaction to the shot is not the same as being clinically sick from the virus and requiring hospitalization. 23andMe scientists sought to describe and characterize this wide range of reactions to the COVID-19 vaccines.
Here are some of the key findings:
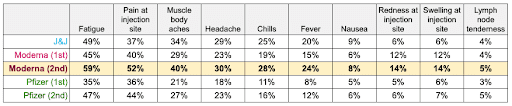
The second Moderna shot seemed to produce the strongest reactions
Compared to the other vaccines, it was those people with a second dose Moderna vaccination who most often reported experiencing any symptoms (85%), and most often reported feeling either very or extremely sick (18%) after their vaccination. Again, these differences were not related to clinical outcomes. In other words, these are relatively modest reactions to the vaccines, but the vaccines still offered strong protection against the virus. In addition, these reactions were generally only for a couple of days after the vaccination. Whereas the severity of COVID-19 infections includes potential weeks or months of hospitalization or death. In addition, scientists still don’t fully know the timeline for so-called COVID-19 “longhaulers,” people dealing with lingering symptoms long after being infected.
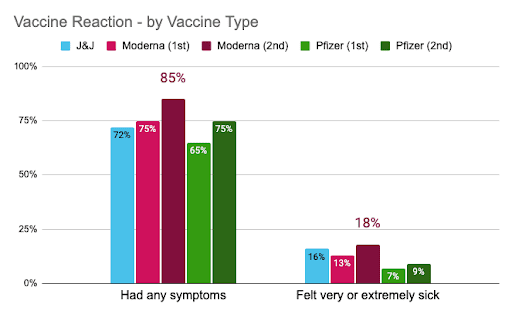
Fatigue, pain at the injection site, and muscle/body aches were the most commonly reported symptoms for all vaccine types. Yet, for every symptom (except nausea), a larger portion of Moderna’s second-dose recipients reported experiencing that symptom compared to recipients of other vaccines.
And in logistic regression models controlling for key demographics (age, sex, BMI, ethnicity, education, and history of COVID-19 infection), having received a second Moderna shot was significantly associated with 3x odds of experiencing any symptom and nearly 1.5x odds of feeling very or extremely sick (as compared to J&J).
So, you are not imagining things — if you got the Moderna 2nd dose and felt “under the weather”, you are not alone. A lot of people did (nearly 1 in 5), but for 94.1% effectiveness against COVID-19, we are all applauding those of you who suffered through a few days of discomfort for your and the greater good.
A history of COVID-19 infection associated with feeling sicker
You may have heard the rumor that people who have had COVID-19 are more likely to feel sick after receiving a vaccine. According to 23andMe data, that seems to be true — a larger proportion of consented research participants previously infected with COVID-19 reported feeling sick for every degree of sickness (from “a little” to “extremely”) compared to those not previously infected with COVID-19. In fact, only a third of participants with a previous infection experienced no symptoms from their vaccine, compared to half of those without a COVID-19 history.
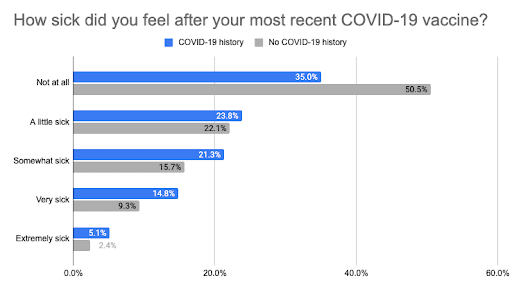
Even after controlling for the key demographic variables listed above, having a history of a COVID-19 infection increased your odds of experiencing any symptoms or feeling very/extremely sick after your vaccination, both by about 30%.
More and stronger reactions for women and younger individuals
Women were more likely to have any symptoms, have more whole body (systemic) symptoms, and generally feel sicker following their vaccination compared to men.
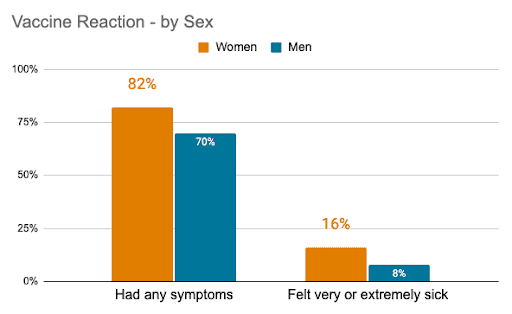
In fact, after controlling for potential confounders, women were almost twice as likely as men to have felt very or extremely ill.
Similar trends were observed for younger individuals when compared to older folks. Those 40 years of age and younger experienced between 2 and 3 whole-body symptoms on average, and nearly a quarter felt very or extremely sick. By contrast, those at least 75 years old experienced between 0 and 1 whole-body symptoms on average, and only 4% felt very ill.
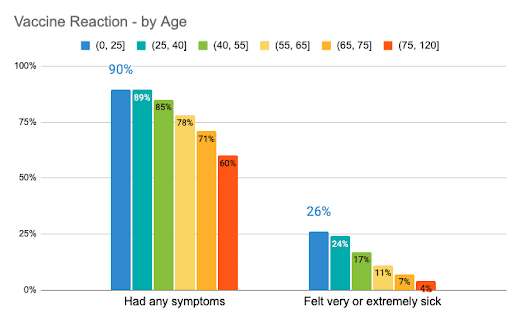
These relationships between sex, age, and vaccine reaction held up, even after controlling for potential confounders.
How do the COVID-19 vaccines work?
The COVID vaccines teach your immune system to recognize and respond to the virus that causes COVID-19. The vaccines introduce genetic instructions to make a harmless protein that is unique to the virus. This triggers a two-step immune response: a first, more immediate and non-specific reaction (the innate immune response), followed by a more gradual, pathogen-specific reaction (the adaptive immune response).6
But why do some people feel very sick from their COVID-19 vaccine, and others don’t feel sick at all? Scientists aren’t quite sure why that is. However, data points to the immune system.
What does my vaccine reaction mean?
Trends identified in 23andMe data support what the vaccine clinical trials and other studies have observed — that certain groups of people are more likely to have felt sicker from their COVID-19 vaccination. These include:
- Women7
- Younger people7, 8,9,10
- Recipients of a second dose vaccine (compared to their first dose)8,9,11
Women, for instance, seem to have stronger immune reactions than men. Research for other types of vaccinations, such as for influenza, yellow fever, and hepatitis, showed that women produce more infection-fighting antibodies than men following vaccination.12 Hormonal and genetic differences between the sexes may also play a role in how the immune systems of men and women respond differently to vaccinations. 12,13
As we age, our immune systems tend to weaken.14 This may explain why younger adults were generally more likely to report a larger number of and more severe symptoms following their vaccination compared to older adults, as seen in data from 23andMe consented research participants and elsewhere, including the vaccines’ clinical trials.7,8, 9, 10
By the time you receive a second dose, your body has already become primed to recognize and respond to the virus that causes COVID-19, and as a result your immune system responds faster and stronger. 15,16 This likely explains why people tend to have more severe reactions to their second dose compared to their first dose.
And it may also be why 23andMe researchers observe that people with a history of COVID-19 infection also feel more ill following their most recent vaccination, compared to those without a prior infection. The virus itself is an additional trigger for your immune responses to kick in. Several small studies have found that people with a history of COVID-19 infection experienced symptoms more frequently17,18 and had higher levels of antibodies after a first dose,19 compared to those without a history of infection.
This analysis on over 100,000 individuals builds upon these findings, showing that a previous COVID-19 infection might not just be related to the number of symptoms experienced following a COVID-19 vaccination, but also the severity of these symptoms.
The COVID-19 vaccines are still effective, regardless of your vaccine-related reaction
Although there is some uncertainty regarding why some people experience more mild or severe symptoms following their COVID-19 vaccination, what we do know is this: the COVID-19 vaccines are effective, whether or not you felt sick after the vaccination.
Data from the vaccine trials showed that not everyone reported vaccine-related reactions; 23% from Pfizer, 18% from Moderna (second dose), and between 39% (younger adults) and 55% (older adults) from J&J didn’t experience any systemic reactions.8,9,10 And this is coming from the same data that demonstrated how safe and effective these vaccines are.
Put another way: “Even if you don’t have an unpleasant reaction, the vaccines are still doing their job, because the real work of the immune system – and of the vaccines – takes place during the second, or adaptive phase of the immune response.”16
What’s next?
Research is ongoing to understand why reactions to the COVID-19 vaccines differ and what these differences mean. This work is part of our ongoing broad research into COVID-19 that has included studying how genetics plays a role in both the susceptibility and severity of COVID-19 and looking at other aspects of the pandemic like its impact on sleep, physical activity and how it has hit some communities harder than others. As part of this work, our scientists are preparing to run genetic analyses to help answer why individuals react differently to the vaccine and what those differences might mean.
*The 23andMe COVID-19 research team includes Adam Auton, Adrian Chubb, Alison Fitch, Alison Kung, Amanda Altman, Andy Kill, Anjali Shastri, Antony Symons, Catherine Weldon, Chelsea Ye, Jason Tan, Jeff Pollard, Jey McCreight, Jess Bielenberg, John Matthews, Johnny Lee, Lindsey Tran, Maya Lowe, Michelle Agee, Monica Royce, Nate Tang, Pooja Gandhi, Raffaello d’Amore, Ruth Tennen, Scott Dvorak, Scott Hadly, Stella Aslibekyan, Sungmin Park, Taylor Morrow, Teresa Filshtein Sonmez, Trung Le, and Yiwen Zheng.