A look by researchers of 23andMe’s internal data from customers who consented to participate in research reveals that some gut health issues affect females differently than males and that these conditions have a bigger impact on people of some ethnicities than others.
The insights come from 23andMe internal data regarding two relatively common gut health conditions, irritable bowel syndrome (IBS) and diverticulitis. The findings confirmed what we already know about common gut health issues and their importance in overall health. It also highlights that genetics plays a big role in the likelihood of developing one of these conditions.
The data shows that the prevalence of these conditions is more common within some ethnicities. Beyond that, certain genetic variants can increase an individual’s risk compared to others of the same ethnicity. Noting the role that ethnicity and genetics play would be important considerations in assessing an individual’s likelihood of developing either IBS or diverticulitis.
This snapshot of 23andMe data from customers who consented to participate in research looks at just two of the many digestive conditions related to gut health, but they are two conditions that impact millions of people worldwide.
The 23andMe Data on IBS
In the case of IBS, estimates are that it impacts between 25 and 45 million people in the US alone, and it impacts females at a much higher rate. Symptoms often include abdominal pain, cramping, bloating, and changes in bowel function, including diarrhea, constipation, or both.
A study published in Nature in late 2021 found that IBS symptoms may be caused by the same biological processes that trigger anxiety, depression, and insomnia. It’s not that IBS causes anxiety or mood disorders but that certain genes are involved in the progression of these conditions. Several studies also indicate that these conditions impact females more than males.
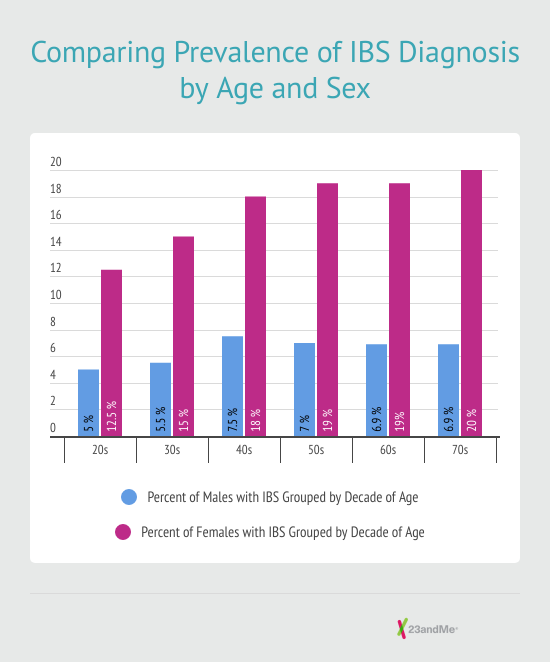
According to data from 23andMe, females are about two and a half times more likely to develop the condition than males. (See figure that compares males and females with IBS by age.) While it’s well documented that sex can impact the likelihood of an individual’s likelihood of developing IBS, far less is known about the role genetics play in this common condition.
Perhaps even more than sex differences, ethnicity and genetics impacts the likelihood of developing IBS. According to new modeling done by 23andMe scientists, both genetics and ethnicity have a big impact on the likelihood of an individual being diagnosed with IBS. In some cases, they present a much bigger risk than previously published non-genetic factors.
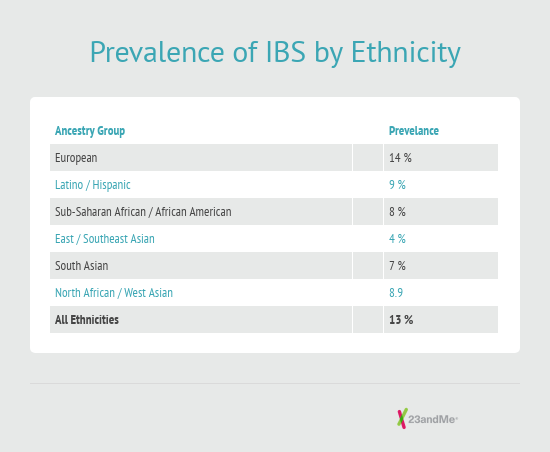
In looking at ethnicity, people with largely Latino or largely European ancestry have the highest likelihood of developing IBS compared to those of other ethnicities. For example, people with mostly European ancestry are almost three times more likely to develop IBS than those of mostly East Asian ancestry.
Statistical Modeling
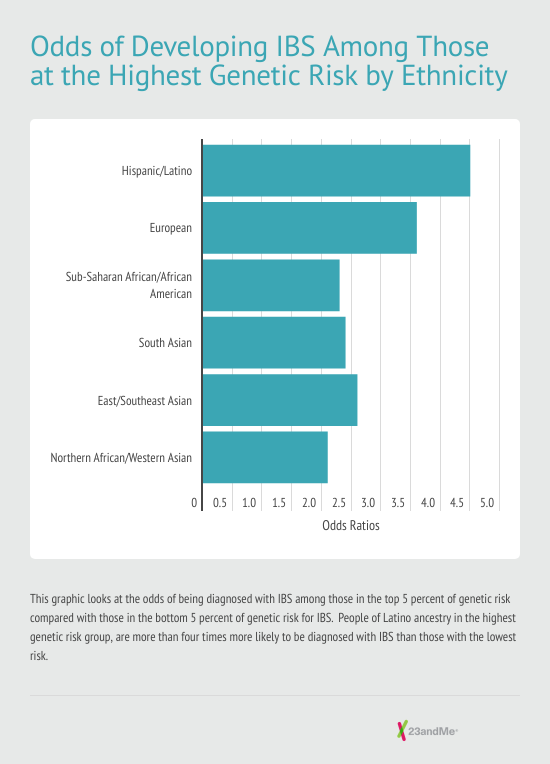
When researchers stratified the data and looked at individuals with a higher genetic likelihood of developing IBS — based on statistical modeling that used more than 12,000 genetic markers associated with IBS — compared to those with the least likelihood, the differences were stark.
For example, people with predominantly Latino ancestry who also were in the highest genetic likelihood* category for IBS are four and a half times more likely to be diagnosed with IBS than Latinos with the lowest genetic likelihood.** If you look at people with primarily European ancestry who are also in that higher genetic likelihood category,* they were more than three and a half times more likely to be diagnosed with IBS than people of European ancestry at the lowest genetic likelihood.**
Why is this distinction important?
Because it shows the outsized impact that genetic factors play on the likelihood of IBS. If you were to graph the polygenic risk for IBS, you’d see a bell curve distribution. Most people would have an average risk or be in the middle of that curve. But at the ends of this curve would be those with the least risk and the most risk.
For those with the highest genetic likelihood* — in the top five percent — the odds that they may develop IBS are quite high when compared to those at the lowest likelihood.** That information on their genetics could be very important for them and their provider in managing their health.
23andMe Data on Diverticulitis
23andMe’s data on diverticulitis confirms some of what we already know but also offers up a few surprises.
As with IBS, both ethnicity and genetics play an important role in the likelihood of developing diverticulitis. While it is relatively common, many people don’t know much about diverticulitis.
It occurs in the intestinal tract, where weak sections of the intestines lead to small bulges or pouches that become inflamed. These pouches, most often found in the large intestine (also called the colon), are called “diverticula.” They are common, especially as we age, but do not cause problems.
It’s estimated that more than half of people in the United States over 60 have diverticula and most likely never have any issues. But fewer than five percent of those individuals will develop inflammation in these pouches, a condition called “diverticulitis,” according to the National Institutes of Health. This can lead to symptoms such as abdominal pain, vomiting, fever, constipation, or diarrhea. More serious complications, such as blockages or perforations, can lead to hospitalization.
Diverticulitis and Ethnicity
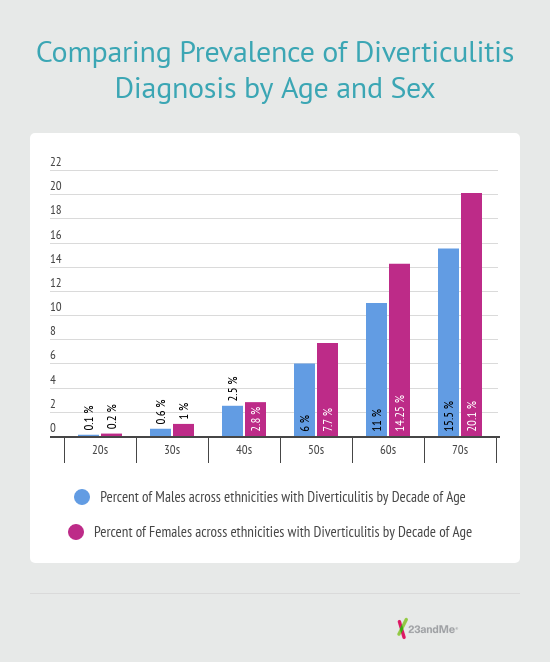
While females were more likely to have been diagnosed with diverticulitis, the difference between males and females was less profound than that for IBS. And in the case of diverticulitis, the likelihood of developing the condition increases considerably as people age, according to the data.
People of European ancestry had the highest prevalence for diverticulitis and those of South Asian ancestry the lowest among individuals we studied.
Looking at genetic likelihood of developing the condition, 23andMe data indicates that people with North African ancestry and Western Asian ancestry (Arabs, Kurds, Persians, and people from Anatolia for example) with the highest genetic risk* for being diagnosed with diverticulitis are about seven times more likely to be diagnosed with diverticulitis than those with the lowest genetic risk.**
People of mostly European ancestry with the highest genetic risk* are five and a half times more likely to be diagnosed with diverticulitis based on their genetics than those with the lowest genetic risk.** People with mostly East or Southeast Asian ancestry who are at the highest genetic risk* for diverticulitis are five times more likely to be diagnosed with diverticulitis than those with the lowest genetic risk.**
Wrapping Up
This snapshot of 23andMe data on two gut health conditions reveals something many haven’t fully understood. It’s not just that genetics plays an important role in risk, but a person’s genetics together with their ethnicity matter.
*Highest risk category: 5% of a given ethnicity, for example, Latino, with the highest genetic risk of being diagnosed with a condition
**Lowest risk category: 5% of a given ethnicity with the lowest genetic risk of being diagnosed with a condition.




