This time last year, pre-pandemic, 23andMe brought together a panel of inspiring women to raise awareness about breast cancer.
The message was clear. Knowledge — about risks, treatments, and the resources available to help — gives you the power to take charge of your health. It’s a message that goes well beyond those who face breast cancer. A lot has changed during the last year. But if we’ve learned anything from this pandemic, it’s that knowledge can empower you to stay healthy.

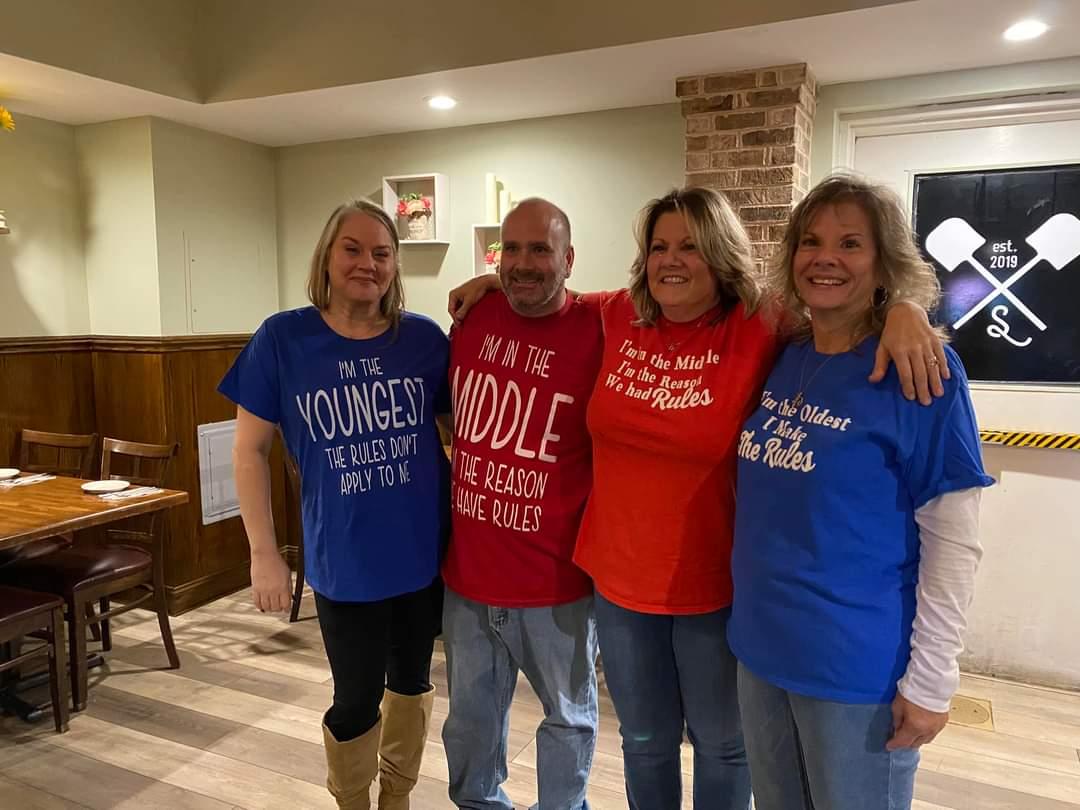
Laura speaking at 23andMe during a panel discussion last year on Breast Cancer Awareness.
So, this year for Breast Cancer Awareness Month, we reached out to one of those women, Laura Osman. Laura spoke so courageously about learning of her own genetic risk for breast and ovarian cancer after getting her BRCA1/BRCA2 (selected variants) Genetic Health Risk report* from 23andMe. Her story offers a lesson to all of us. She faced her risk head-on, consulted with her doctor, and took action for her health.
Laura, a healthy mother of three and a former All-American middle-distance runner, was stunned. Her 23andMe reports indicated she had a variant in the BRCA1 gene that put her at an elevated risk of breast and ovarian cancer.
“At first, when I saw it, I thought it was a mistake,” she said.
It wasn’t just that she took good care of herself. Laura also knew that none of the women in her family had had breast or ovarian cancer. On top of that, with each of her pregnancies, Laura and her husband had gone through something called the JScreen. This genetic test looks specifically at genetic conditions that are common among people of Ashkenazi Jewish ancestry. The screens help inform prospective parents about the risk of passing on genetic conditions to their children. There wasn’t anything found when she did that screen.
Laura was so sure she didn’t have anything to worry about genetically that she was mostly focused on her 23andMe Ancestry reports when she got her results. She wanted to know if perhaps she had some hidden Swedish ancestry that would explain her blond hair. (It turned out she was 99 percent Ashkenazi Jewish.)
So, it was an utter surprise when looking at her 23andMe’s BRCA1/BRCA2 (Selected Variants) Genetic Health Risk report* she saw she carried one of the variants 23andMe tests for. 23andMe’s report looks at just three variants among the thousands of mutations that contribute to cancer risk. These variants are found mostly in people of Ashkenazi Jewish ancestry. But they are among the most well-studied variants and convey significant risk. No matter one’s ethnicity, having one of them increases the risk for breast and ovarian cancer by 45 percent to 85 percent by the age of 70.
But many individuals who carry a BRCA1 or BRCA2 variant don’t have a family history of cancer. 23andMe research found that about 44 percent of individuals with specific BRCA1 or BRCA2 variants did not have a first-degree family history of BRCA-related cancer. Several studies have shown that as many as 50 percent of people with one of these mutations wouldn’t qualify for breast or ovarian cancer screening under current medical guidelines.
“The 23andMe report said consult with your doctor, so that’s what I did,” Laura said.
Her doctor ordered follow-up genetic testing. He deduced that she’d inherited the risk variant from her father, who’d battled prostate cancer. Laura knew this was serious; carrying the mutation put her at a much higher risk for both ovarian and breast cancer. It was hard to get her head around what to do next.
“My body, which I have always viewed as healthy and strong … was a ticking time bomb,” she said. “(But) I knew fear and feeling sorry for myself was not an option.”
She reached out first to friends, then to a national nonprofit called Sharsheret, which works with Jewish women living with or at increased genetic risk for breast or ovarian cancer. The group offered resources and helped connect her with other women who faced similar risks. Several years ago, 23andMe conducted a smaller study looking at the response to unexpected BRCA findings. That study found that those who learned they carried a risk variant generally took appropriate actions, talking to their doctors and sharing their results with family members, creating what the study called a “cascade effect” that benefited relatives who might not know of the family risk for these hereditary cancers.

Laura with her husband and three young children.
In Laura’s case, she wanted to hear from women who chose to have surgery to remove their breasts and ovaries. She wanted to know as much as she could about what to expect if she made that decision. Laura talked more to her doctors and carefully weighed her options.
“I think it might be much harder for someone who hasn’t had children yet,” she said. “It’s so different for me because I’d had my children, but we need to support women whatever their choices.”
Within five weeks of receiving her 23andMe reports and after undergoing clinical testing recommended by her doctor, Laura underwent the first of what turned out to be three surgeries to remove her ovaries and breasts.
“It wasn’t easy,” she said.
It took a few weeks before she could lift her young daughter and about a month and a half before she was running again. More than a year later, she is back to racing and is doing fine.
“I am not sure I will ever be able to repay the gratitude I have for 23andMe,” Laura said. “(It’s allowed) me to hopefully stop cancer before it could stop me.”
*The 23andMe PGS test uses qualitative genotyping to detect select clinically relevant variants in the genomic DNA of adults from saliva for the purpose of reporting and interpreting genetic health risks, including the 23andMe PGS Genetic Health Risk Report for BRCA1/BRCA2 (Selected Variants). Your ethnicity may affect the relevance of each report and how your genetic health risk results are interpreted. The test is not intended to diagnose any disease and does not describe a person’s overall risk of developing any type of cancer. It is not intended to tell you anything about your current state of health, or to be used to make medical decisions, including whether or not you should take a medication, how much of a medication you should take, or determine any treatments. Warnings & Limitations: The 23andMe PGS Genetic Health RIsk Report for BRCA1/BRCA2 (Selected Variants) is indicated for reporting of the 185delAG and 5382insC variants in the BRCA1 gene and the 6174delT variant in the BRCA2 gene. The report describes if a woman is at increased risk of developing breast and ovarian cancer, and if a man is at increased risk of developing breast cancer or may be at increased risk of developing prostate cancer. The three variants included in this report are most common in people of Ashkenazi Jewish descent and do not represent the majority of BRCA1/BRCA2 variants in the general population. This report does not include variants in other genes linked to hereditary cancers and the absence of variants included in this report does not rule out the presence of other genetic variants that may impact cancer risk. The PGS test is not a substitute for visits to a healthcare professional for recommended screenings or appropriate follow-up. Results should be confirmed in a clinical setting before taking any medical action.