With apologies to Walt Whitman, we all contain multitudes … of microbial cells, trillions of microorganisms that live in and on our bodies.
The human microbiome is vast and varied and accompanies us through our lives, changing as we age. As scientists continue to learn more about these microscopic ecosystems on our skin, mouths, and gut, we understand more and more about the sometimes surprising role they play in our health.
Researchers at 23andMe, in collaboration with the Michael J. Fox Foundation, recently published a study in Communications Medicine looking at the gut and oral microbiome of people with Parkinson’s disease. The study offers intriguing new insights that could help diagnose and monitor disease development and progression earlier.
“To our knowledge, this is the largest single study to test the relationships between both the oral and gut microbiomes and Parkinson’s disease, providing us with the statistical power to uncover potentially important associations,” said Keaton Stagaman, PhD, a postdoctoral research scientist at 23andMe and a co-author of the study.
Gut-Brain Axis
Parkinson’s is a neurodegenerative disorder that affects movement and cognitive function. Research has found a strong ‘gut-brain axis’ that connects the central nervous system to the gastrointestinal tract, and studies have recently pointed to the potential link between Parkinson’s disease and the gut microbiome.
Along with Parkinson’s, changes in the gut microbiome have been linked to other conditions, including inflammatory bowel disease, Clostridium difficile infections, autoimmune disorders, diabetes, and obesity. The links are intriguing but not yet fully understood. That said, a better understanding of the microbiome and its role could be essential for diagnosing and treating many conditions.
The new research by 23andMe offers more evidence of the connection between Parkinson’s and changes in the gut microbiome.
Different Types of Microorganisms
For this study, scientists used microbiome data from saliva and stool samples of people with and without Parkinson’s disease.
Scientists have identified about 1,000 microbial species in the human mouth, whereas the human gut has the densest collection of microorganisms in the body. According to the National Institutes of Health, the large intestine has as many as 100 billion to one trillion cells per milliliter and is among the densest microbial ecosystems ever observed.
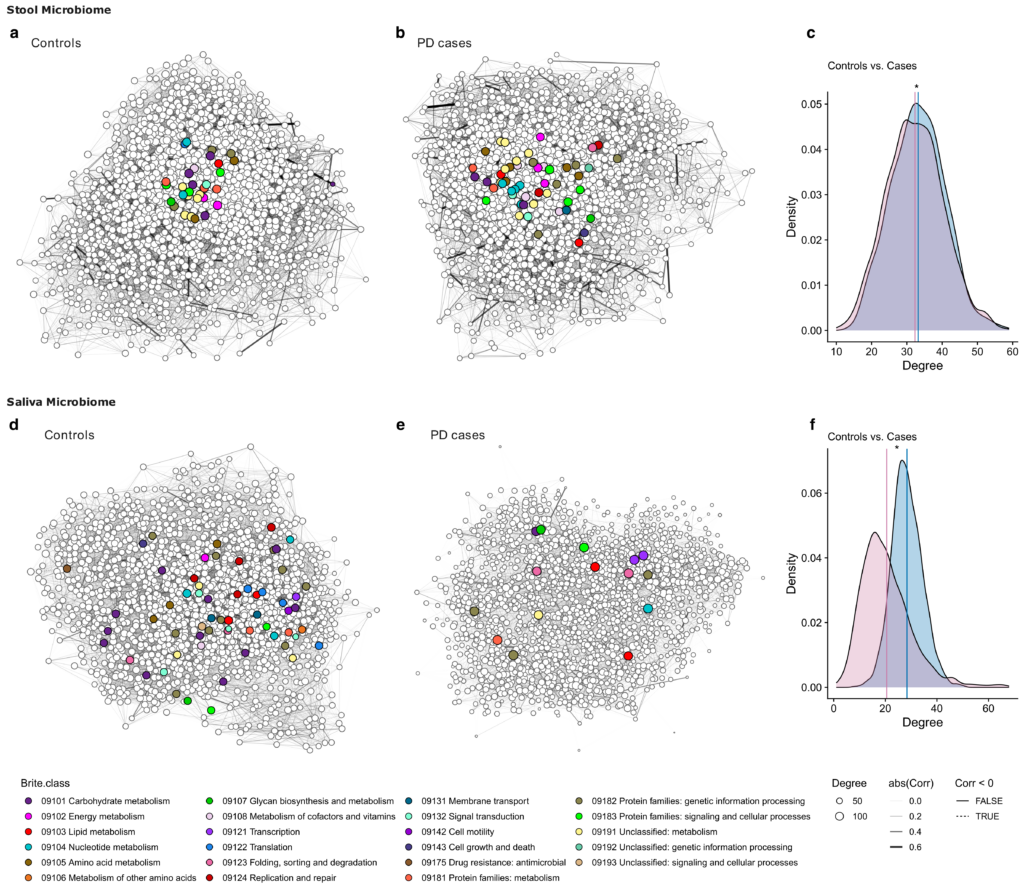
Because of the vast number of different microorganisms, 23andMe scientists in this research used sequence data to group those organisms into Operational Taxonomic Units or closely related types of bacteria. Using these groupings, the scientists were able to find significant differences in the type and abundance of microorganisms in the microbiome of people with Parkinson’s when compared to those without the disease.
This was the case in both stool and saliva samples. This is significant and suggests that using saliva samples, which are much simpler for patients and scientists to collect, is adequate for detecting differences in the microbiome for those with Parkinson’s.
The Findings
In undertaking the study, the researchers thought there might be distinct microbial changes in people with Parkinson’s and that those changes could be seen in the early stages of the disease before many symptoms develop.
Among the signature differences researchers found was a higher diversity of microbes within the microbiome of those with Parkinson’s. This was the case even when considering other things that could affect the diversity of microbes, such as oral hygiene or constipation. In addition, the researchers said that the amount and diversity of microbes in samples was a good predictor of whether someone had Parkinson’s disease. Using a well-known machine learning algorithm called Random Forest, the team could predict whether a person had Parkinson’s or not 80 percent of the time.
The researchers also identified specific types of bacteria that differed between people with Parkinson’s and those who did not have the disease. The scientists believe that the findings might help find specific markers in the microbiome, specifically in saliva samples, that could be used to monitor for early signs of the disease.
Other studies have shown that changes in the gut microbiome may offer early indications of the onset of changes in a person’s motor functions.
Learn More
Beyond the ability to use a person’s microbiome to evaluate the status of Parkinson’s, the paper also suggests that altering a person’s microbiome may offer another avenue for treating Parkinson’s symptoms.
You can read the complete study in Communications Medicine here.
Additionally, data from the Fox Insight PD Microbiome sub-study are available to qualified researchers here.