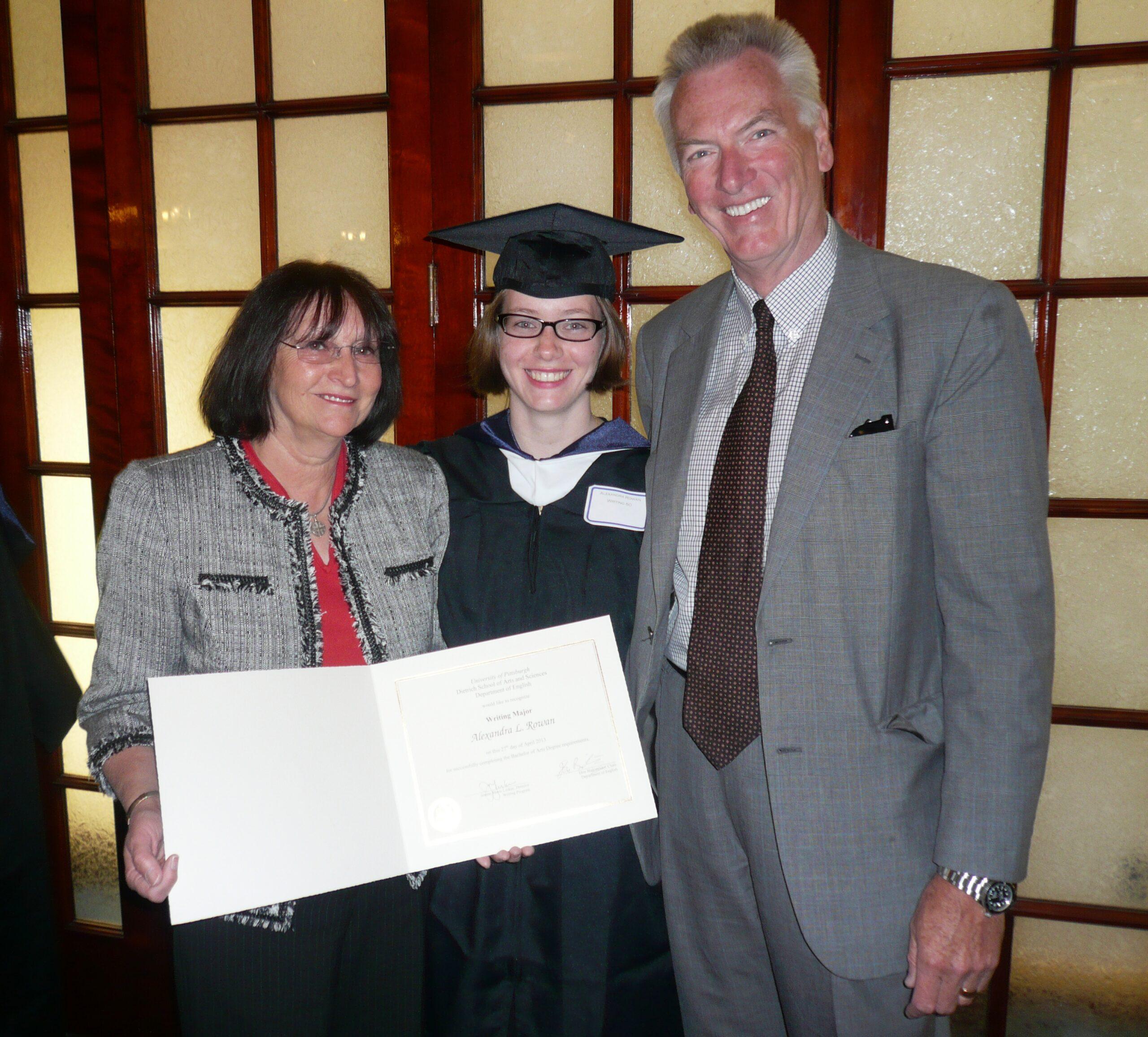
David and Roz Rowan recently spent some time with us here at 23andMe to talk about how their foundation started after the death of their 23-year-old daughter Alexandra, who died after suffering a massive pulmonary embolism or blood clot in her lung in 2013.
Like every parent who has lost a child, David and Roz lived with an inconsolable sense of loss, but they channeled their grief to form the Rowan Foundation and to raise awareness about preventable blood clots like the one that claimed their daughter’s life.
Since its founding, the Rowan Foundation has focused on drawing specific attention to the risk of blood clots and stroke in women’s reproductive health, especially risks linked to estrogen and estrogen-based contraception. Many people are unaware of the risk of blood clots, which can happen to anyone and can be further compounded by genetics. Two of the most common genetic variants linked to hereditary thrombophilia, or the genetic health risk for harmful blood clots, are found within the F5 and F2 genes.* A specific variant in the F5 gene is referred to as factor V Leiden, and someone with this gene variant has a significantly increased chance of developing venous thromboembolism (VTE) or blood clot in a vein. For women who have a genetic predisposition toward clotting, taking estrogen-containing birth control compounds their clotting risk. For example, women who are affected by factor V Leiden and who also use combined hormonal contraception substantially increase their risk for clotting, according to some studies. Unfortunately, many people with a genetic predisposition for blood clots, as well as many women using combined hormonal birth control, only learn of their increased risk after experiencing a clot.
Since her death, Alexandra’s mom, Roz, learned that she carries the factor V Leiden variant and has also suffered from a series of clots, first in one of her legs, then in a lung. In 2022, a clot triggered a stroke. David and Roz believe that Alexandra likely, too, had the variant. If she had known her genetic status, she may have decided against using estrogen-based birth control.
Alexandra’s Story
23andMe: Thank you so much for taking the time to talk with us about your daughter and the work of the Rowan Foundation. The aim of your work is to help prevent other women like Alexandra from dying due to preventable blood clots. Is simply raising awareness about blood clotting risk the focus of your actions?

David: The work of our Foundation is intended to honor our daughter Alexandra’s memory and is focused on increasing awareness about the risks for dangerous blood clots that women face throughout their lifetime. Given Alexandra’s experience, we’re particularly focused on risks linked to estrogen-based contraception options – including the pill, patch, or ring – that are known to raise clotting risks.
We’ve created a spectrum of educational resources and tools that provide important information about clotting and women’s reproductive health and are intended to help women make fully informed decisions about their birth control options. Contraception decision-making involves many factors and can be confusing or overwhelming when considering the many available options.
Birth control is a very personal decision; it’s a woman’s choice. Our mission focuses on helping women make a choice that is effective and safe, given their personal preferences and health history. We want to do all that we can to help mitigate death and injury due to blood clots and, ultimately, to help save lives.
Understanding Risks and Knowing Symptoms
23andMe: Roz, you have now had a series of blood clots— one most recently that led to a stroke. What can you tell us or other women about symptoms and ways to prevent clots? What kinds of discussions about blood clots should we have with our primary care providers, gynecologists, and other healthcare providers?
Roz: Shortness of breath was the only symptom I had before my deep vein thrombosis or the blood clot in my leg. Similarly, I had difficulty breathing when I experienced a pulmonary embolism or blood clot in my lung. The only symptom our daughter Alexandra mentioned was a pain in her thigh, which she assumed was a pulled muscle.
That’s the thing with blood clot symptoms: They can be somewhat elusive because they mimic the symptoms of other ailments and can be dismissed or misdiagnosed as other things, like asthma, anxiety, or muscle strains, for example.
It’s important to know that not everyone will experience the same symptoms, and some people will experience no symptoms. In fact, we’ve learned since Alex died that sudden death is the first symptom in about 25 percent of people who have a blood clot in their lungs.
When symptoms do occur, they might include soreness, swelling, and red or discolored skin if the person has a blood clot in their leg or arm. When a blood clot forms in a person’s lung, the most common symptoms are shortness of breath, coughing, and chest pain.
The Foundation has created a number of resources to help people understand and remember blood clot symptoms, as recognizing these signs and symptoms can save lives.
You asked about the best way to prevent clots, and the first thing I would suggest is that everyone should know their own risk – people should discuss all of their risk factors with their healthcare providers. Some of the significant risk factors for clotting, in addition to estrogen-based birth control, are pregnancy, surgery, hospitalization, cancer, genetic or inherited clotting conditions, and being immobile or not moving for lengthy periods of time.
The best first step in preventing dangerous clots is to know your personal risks and recognize signs and symptoms.
Knowledge is Power
23andMe: We have heard from 23andMe customers who have had two different kinds of experiences with learning their genetic health risk for Hereditary Thrombophilia* – either that they discovered they had factor V Leiden using 23andMe and didn’t have a history of blood clots or that they discovered their increased genetic risk for clotting after suffering from a blood clot. One customer, Jessica Diaz, had a stroke at 36. She, too, carried a genetic risk but didn’t learn about it until after her stroke. It stunned her that this kind of risk was not more common knowledge. Why do you think that is the case, and what can be done about it?
David and Roz: Information and knowledge are key components in personal health and well-being. It may be an old saying, but it’s true: Knowledge is power.
Certain genetic clotting conditions, however, are not common or not fully understood. Not everyone who has a genetic clotting condition will experience a clot and can go their entire life unaware they have this underlying condition. However, for those who experience a clot, it is frequently the first time they learn of their condition.
Given our family’s experience, we see the emerging promise for genetic testing to help people learn more about their health history and to leverage the terrible and, at times, deadly “surprise” factor associated with clotting disorders. Armed with this type of information, people can make decisions with their healthcare providers to help preserve and protect their health.
The Broader Impact
23andMe: The Rowan Foundation shares stories from other women who have suffered from clots. What is uncanny about each is how many women who have gone through this were unaware of the risk. While these clots can be life-threatening, some of those who survive still live with longer-term health issues. Can you talk about that?
DAVID: Venous blood clots impact about one million people in the United States each year, and about 100,000 of these individuals will lose their life to a blood clot this year.
The toll of blood clots, however, continues even among those who are fortunate to survive. Many people who experience a blood clot will suffer from respiratory issues after a pulmonary embolism, and this can impact their lives and livelihoods dramatically. We know of strong, athletic individuals who experienced a blood clot that left them with impaired lung function that made it difficult for them to even just get out of a chair and walk across the room. Also common are complications like post-thrombotic syndrome, or physical discomfort and even disability due to the vascular damage that blood clots in the legs can cause.
The death and disability associated with blood clots add up to a public health burden that needs to be addressed more effectively, and it’s our hope that any work we do to help raise awareness will help to reduce this burden.
Hormone Therapies
23andMe: When most people hear about hormone therapies, they might think about oral contraceptives for females of reproductive age. However, there can be many other reasons why a person might use estrogen-based hormone therapies throughout their lifespan – for example, during menopause for symptom management, after menopause to treat or prevent osteoporosis, during specific breast cancer treatments, or during gender-affirming hormone therapy for transgender women. How do you think our communities can better raise awareness about who should know their risk for blood clots and when it might be especially important to be aware of that risk?
ROZ: Women face a continuum of blood clot risks throughout their lifetime, and we should be provided with potentially life-saving information and education about these risks at an early age or whenever we encounter this type of medication or therapy.
For example, many young women are first prescribed estrogen-based birth control when they go away to college and seek contraception from their university health center. We have heard numerous stories from families who lost their daughters like we did after they were first prescribed estrogen-based birth control in this way. Clear and relatable information should be shared with young women about this risk. Any tools that can help inform women of a potential for increased risk due to a genetic or inherited clotting disorder should be an option for them to consider or access.
We feel so strongly about this that the Rowan Foundation implements educational programs and distributes resources focused on this audience each year. In fact, we’ve done extensive educational outreach on university campuses nationwide to get information about dangerous blood clots into the hands of young women who might be considering their contraception options for the first time.
We need to tailor and make our educational efforts about clotting resonate effectively with women so they can learn about the risks and the signs and symptoms of blood clots and protect their health.
Pregnancy and Postpartum
23andMe: There’s been lots of recent news attention placed on maternal mortality rates in the United States and the instances of preventable deaths during pregnancy and postpartum. Can you speak on how knowing your risk for blood clots might be relevant to pregnancy, birth, and the postpartum period?
ROZ: Pregnancy is a major risk factor for clotting and one of the most common causes of pregnancy-related deaths in the United States. The greatest risk for pregnant women occurs in the weeks after the baby is born. Clotting poses a risk not only to the mother but also to the developing baby.
If a pregnant woman has a known clotting disorder, her clotting risk increases dramatically. Knowing your genetic predisposition for clotting when pregnancy is planned or during pregnancy can be life-saving. There are treatments available that can help to safely prevent blood clots during pregnancy and that will not harm the developing baby.
Women should talk to their doctors about this risk and make sure that they have some type of blood clot prevention plan in place as they go through pregnancy and their delivery date approaches.
Not Just Women at Risk
23andMe: We know blood clots can impact anyone, not just females. What do you hope that a male with a genetic risk for clotting, like factor V Leiden, might hear from his healthcare team about preventing blood clots, both for him and for his at-risk family members?
David: It’s interesting. We are focused on women’s health and clotting, and we know that there are life stages that pose clotting risks that are specific to women—like family planning and birth control, pregnancy and childbirth, and the treatment of menopause symptoms with hormones later in life. However, more men than women actually experience clots, and men need to be tuned into their clotting risks, too.
We think that any person diagnosed with a genetic clotting disorder has information that could help save their life and also protect the health of their loved ones. Suppose that person and their family members know they are at increased risk for clotting. In that case, they have the vital information they need to prevent clots, whether using some type of anticoagulant medication or reducing other clotting risks by staying active and maintaining a healthy weight.
Not every person diagnosed with a clotting disorder will experience a clot, and the diagnosis may make little to no difference in their day-to-day life. However, armed with the knowledge that they are genetically predisposed to clotting, they can take steps to eliminate or minimize other risks and also be vigilant about clotting symptoms.
Looking Out for Signs & Symptoms
23andMe: Looking back at Roz’s experience or Alexandra’s life, were there any indications that a clot was developing? Are there subtle symptoms or lifestyle risks you want to make others aware of?
Roz: Breathlessness led me to seek medical attention on both occasions when I experienced a clot. When I suffered a stroke, the impact was immediate. It was a stunning medical emergency, but there were no subtle signs or symptoms that preceded that experience. Alex had some thigh pain that she assumed was a muscle strain.
From our daughter’s experience, we know that it’s important to always get things checked out. Don’t dismiss anything that you can’t explain or that you don’t understand – no matter how subtle or inconsequential it might seem.
Blood clots frequently start in a person’s legs or arms. Left untreated, they can grow larger or break off and travel to the lungs, where they can be deadly. Getting attention quickly, as when stroke symptoms are experienced, can save your life.
Family Health History
23andMe: Talking about family health history can be sensitive, especially when a family has a tragic health-related event like a sudden death due to a preventable blood clot. What advice do you have for people who want to learn more about their family health history or want to share what they know about their genetic risks but are nervous about how their family will react?
David: I would suggest that anyone who might be nervous about sharing this information should consider how nervous or devastated they might be if they didn’t share that information and someone lost their life. This type of genetic health or family health history should be considered a valuable resource for individuals and their family members.
Raising Awareness
23andMe: Are you also working to raise awareness within the medical community about how they talk to women about their risks or screening for these kinds of risks?
David: Our website houses lots of information about women’s health and clotting, and we recently added important information and resources about genetic clotting conditions and genetic testing too. This information, along with the suite of educational tools and resources we’ve created, can be used by health providers and health educators interested in raising awareness about clotting risks in women’s health.
We’re always exploring ways to improve how we present this information or reach people through programs and educational tools that will resonate strongly with them. In fact, we’re currently planning a conference to bring together experts in this field to explore this issue and to identify the best ways to improve the dialogue between patients and physicians about blood clots.
23andMe: It’s incredible what you’ve done in your daughter’s name and how you are helping other women by raising awareness about this important aspect of women’s health. What do you want people to know about Alexandra?
David and Roz: Alexandra was our only child. When we lost her, we lost the center of our universe. She was a sweet young woman, she loved the outdoors and traveling. She was smart, had just graduated from college, and she had her whole life in front of her when she died suddenly. Alexandra had a bright future in front of her, but that future was dimmed and her promise and potential unfulfilled.
The work of the Foundation has helped us turn our grief into something productive. The work we do serves as a tribute or legacy for our daughter Alexandra and also honors all of the other women like her who lost their lives to preventable blood clots. We want to give voice to their experiences and educate the public so that we can help prevent other families from experiencing this same type of tragic loss.
Note:
†Within this blog, which observes National Women’s Health Week, we use the terms “women” and “woman” to refer to individuals with the capacity for birth, trans women, and nonbinary individuals taking estrogen. Learn more about why we made this decision in this helpful article.
*The 23andMe PGS test uses qualitative genotyping to detect select clinically relevant variants in the genomic DNA of adults from saliva to report and interpret genetic health risks. It is not intended to diagnose any disease. Your ethnicity may affect the relevance of each report and how your genetic health risk results are interpreted. Each genetic health risk report describes if a person has variants associated with a higher risk of developing a disease but does not describe a person’s overall risk of developing the disease. The test is not intended to tell you anything about your current state of health or to be used to make medical decisions, including whether or not you should take a medication, how much of a medication you should take, or determine any treatment. The Hereditary Thrombophilia genetic health risk report is indicated for reporting the Factor V Leiden variant in the F5 gene and the Prothrombin G20210A variant in the F2 gene. It describes if a person has variants associated with a higher risk of developing harmful blood clots. The variants included in this report are most common and best studied in people of European descent. These variants are also found in populations with European ancestry, like African Americans and Hispanics or Latinos.