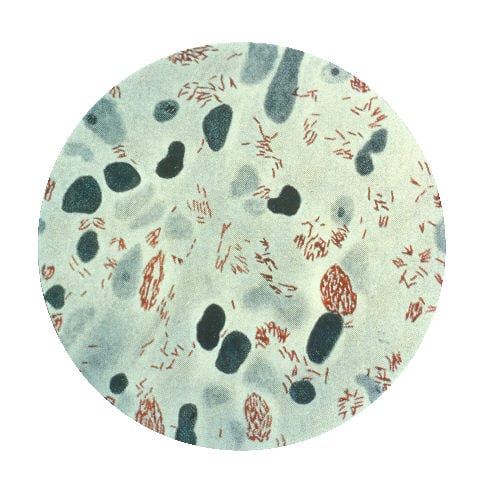
Leprosy is a chronic, disabling disease caused by a bacterium (Mycobacterium leprae) that infects only humans and armadillos.
The disease affects the skin and peripheral nerves, leading to sores, numbness in the limbs, muscle weakness, and, in severe cases, disfiguring nodules on the skin. Known since biblical times, leprosy was highly stigmatized until the latter part of the 19th century when Norwegian doctor Gerhard Hansen discovered that it was caused by a microorganism.
Treatment and Prevention
Although multi-drug therapy has cured millions of people of leprosy in recent decades, hundreds of thousands of new cases still occur per year, mostly in developing countries. Finding a way to eradicate the disease is therefore considered essential for reducing the number of preventable disabilities worldwide.
Because Mycobacterium leprae is specific to humans and cannot be grown in lab dishes, research into factors influencing disease susceptibility and clinical outcomes has been limited. But the host environment, as well as the bacterium itself, can affect the course of the disease; in other words, human genetic factors may play an essential role in determining who is more susceptible to infection.
Since leprosy has been shown to cluster in families, scientists suspect that much of the variability in disease susceptibility and symptoms stems from diversity in individual human immune systems rather than differences between and within strains of the bacteria.
New Research
In a new study published today in New England Journal of Medicine, researchers report new human genetic factors associated with susceptibility to leprosy in Asians. Led by Fu-Ren Zhang of the Shangdong Academy of Medical Sciences in China and Jian-Jun Liu of the Genome Institute of Singapore, the scientists tested 93 variants across an estimated 50 genes in 3254 Chinese individuals with leprosy and 5955 Chinese individuals without the condition. Their analysis identified seven gene variants to be significantly associated with leprosy.
“The discovery of these genes is a major breakthrough for research in leprosy and infectious diseases in general and will be significant in the early diagnosis and development of new treatments,” said Dr. Liu in a press release.
The strongest associations were in HLA-DR-DQ, C13orf31, and NOD2. In addition, some of the genetic variants were more strongly associated with a form of leprosy that results in more severe symptoms, known as the multibacillary form. These included NOD2 and the variant in LRRK2.
Association with Crohn’s
Altogether, five of the seven genes identified in the study could be shown to interact biologically in the context of immune response to infection. Two of these five genes, NOD2 and TNFSF15, harbor genetic variants associated with Crohn’s disease. Crohn’s manifests some common features with leprosy at the cellular level, and other researchers have suggested that mycobacterial infection may be a risk factor for Crohn’s. The findings reported by Zhang and Liu and their colleagues provide additional evidence for shared disease mechanisms between Crohn’s disease and leprosy. They may increase the range of treatment options for both conditions.
** This effect is only applicable to the multibacillary form of leprosy. LRRK2 is better known as a susceptibility gene for Parkinson’s disease (see 23andMe’s report on this condition). Interestingly, PARK2, another gene linked to Parkinson’s, was associated with leprosy in earlier studies. The reason for the connection between Parkinson’s and leprosy is unclear, though researchers have speculated that some of the same treatments may be effective for both conditions.



