New research suggests the primary genetic mutation that causes alpha-1 antritrypsin deficiency, a condition that results in liver damage and a wide variety of other problems, also affects risk for liver disorders associated with cystic fibrosis.
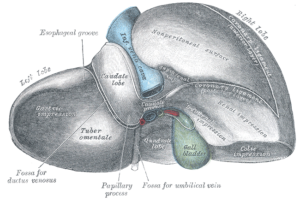
Cystic fibrosis is an inherited, childhood-onset disorder that causes the lungs, intestines and pancreas to become clogged with mucus, resulting in breathing and digestive problems. Between three and five percent of CF patients also experience liver disease, which leads to scarring that can block blood flow through the organ and increase blood pressure in surrounding vessels.
Liver transplants have been necessary in many of these cases, but the new genetic research may be able to help prevent them by enabling prediction and prevention of CF-associated liver disease.
A team of researchers at the University of North Carolina at Chapel Hill, led by Michael Knowles, analyzed genetic variants in five genes that have been proposed to be involved in cystic fibrosis-related liver disease. The study involved nearly 1,000 patients, both with and without liver symptoms.
The results, published last week in the Journal of the American Medical Association, identified one genetic variation that increases a cystic fibrosis patient’s risk of developing liver disease. Researchers found that each T at the SNP increases odds of liver disease in CF patients by 4.17 times. A T at both copies of this SNP causes alpha-1 antitrypsin deficiency.
Researchers are still searching for genetic variations associated with other complications of cystic fibrosis, including lung disease, intestinal obstruction and diabetes. Further studies on severe liver disease related to cystic fibrosis may reveal more risk factors for severe symptoms that can be detected early in life.