By Bethann Hromatka, Ph.D.
HLDL is the “bad” cholesterol that clogs arteries and is linked to coronary heart disease. Although people can do a lot to lower LDL levels and prevent heart disease – eating healthy, exercising, and taking certain medications – it’s also likely that genetics influences the relationship between LDL and heart disease.
For instance, some studies suggest that a particular version of the KIF6 gene called 719Arg may be linked to both heart disease and response to statins, a class of drugs used to lower LDL. The involvement of this SNP in the complex interplay between LDL cholesterol and heart disease, however, is proving to be controversial.
The KIF6 variant came to the attention of researchers when it was suggestively linked to coronary heart disease in 2007. Weak evidence for the association was also reported in a number of prospective studies – people with at least one copy of the KIF6 variant, also called “carriers”, seemed to develop heart disease more than people without this version of the gene (non-carriers). Additional studies suggested that carriers receive greater benefit from statin therapy (pravastatin or atorvastatin) than non-carriers, but overall, none of these reports provided definitive statistical evidence for an association between the KIF6 variant and heart disease.
Based on these initial reports, Celera, a biotechnology company that was involved in many of these studies, developed a genetic test that determines whether a person has the KIF6 variant. This test was devised with the hope that it could pinpoint individuals who would derive the most benefit from statin therapy. Since as much as 60% of people with European ancestry carry at least one copy of this version of the KIF6 gene, millions of Americans with high LDL could potentially benefit from such a test. Although this version of the gene is also fairly common in African Americans and Asians, most of the research on KIF6 has been performed in people of European ancestry.
Although Celera filed for FDA clearance to market the test in early 2011, the application was rejected because there wasn’t enough data to support its safety and effectiveness. This is in part because data surfaced in 2010 that contradicted the original reports. A large study with 56,000 participants showed that people with the KIF6 variant do not suffer cardiac events more than non-carriers and another report suggested that statin therapy had the same effect on carriers and non-carriers.
But like many research stories, there is now another twist. New findings published in PLoS One by lead author Brian Ference confirmed that, on average, the KIF6 variant is not associated with heart disease risk, but then offered novel findings suggesting that people with the KIF6 variant are more vulnerable to the harmful effects of LDL and therefore may be at increased risk for heart disease. This study is the largest meta-analysis of KIF6 to date with 144,931 participants.
In Ference’s study, KIF6 carriers with very high LDL suffered more cardiac events than non-carriers with similar LDL levels and, conversely, carriers who lowered their LDL experienced greater protection from cardiac events compared to non-carriers who lowered their LDL to a similar degree. In addition, people with KIF6 variant benefited more from statin therapies than non-carriers. Carriers on statin therapy experienced a 27% reduction in heart disease risk per mmol/L decrease in LDL, while non-carriers on statin therapy experienced a 17% reduction per mmol/L decrease in LDL.
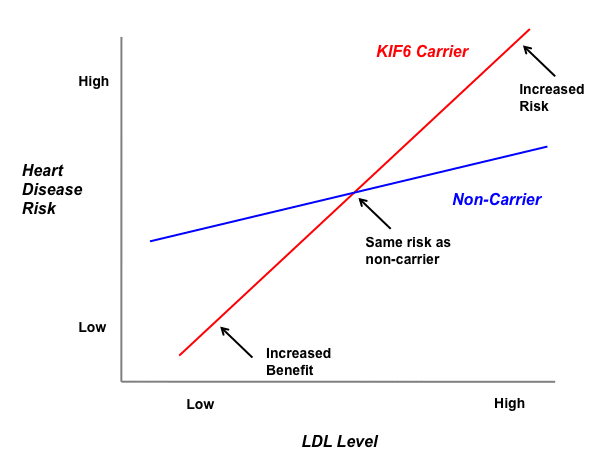 This figure shows a theoretical effect of a genetic variant on heart disease risk dependent on LDL levels. In the case of KIF6, the red line would correspond to carriers and the blue line to non-carriers. KIF6 carriers would exhibit increased heart disease risk than non-carriers at high LDL levels, but would also see a larger reduction in risk from lowering their LDL compared to non-carriers. (Figure adapted from Ference et al (2011).
This figure shows a theoretical effect of a genetic variant on heart disease risk dependent on LDL levels. In the case of KIF6, the red line would correspond to carriers and the blue line to non-carriers. KIF6 carriers would exhibit increased heart disease risk than non-carriers at high LDL levels, but would also see a larger reduction in risk from lowering their LDL compared to non-carriers. (Figure adapted from Ference et al (2011).
These new findings add complexity to the story. They suggest that KIF6 carriers are more susceptible to heart disease risk conferred by high LDL levels but conversely derive greater benefit from lowering their LDL. These LDL-specific effects may help to explain why some of the early, small studies observed a possible link between the KIF6 variant and heart disease when the large study from 2010 – in people with a range of LDL levels – did not. Future studies may add even more clarity.



