As far as disease names go, cancer appears to be pretty simple. Breast cancer is a cancer of the breast, and prostate cancer is a cancer of the prostate.
Although this naming system describes where cancer starts out, it doesn’t tell us much about where cancer will spread, which drugs (if any) will work, if the patient will have a bad reaction to therapy, or whether the patient is likely to survive cancer.
Going Deeper
To understand these questions, we need to drill deeper and analyze the molecular barcode of both the cancer and the host.
Understanding the molecular profile of a cancer cell can help physicians understand which drugs will be effective in treating the cancer.
The underlying code for what the cancer “shows” to the rest of the body and how it will behave in the body depends on the DNA inside the cancer cells. And what’s becoming evident is that cancer is much more complicated than we used to think.
Changes in DNA Underlie Cancer
Cancer develops when normal cells in the body grow and reproduce uncontrollably because of “mistakes” in the DNA code. DNA (a copy of which is contained in each cell) contains finely tuned instructions for cell growth and production, but as cells copy and pass on this DNA they sometimes make mistakes. These mistakes are technically called “mutations” and cause the DNA to be slightly different from the original.
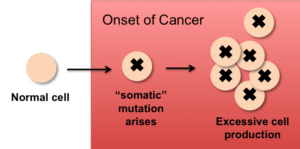
The mutations that make cells grow too much and thereby cause cancer arise in the course of a person’s lifetime (as opposed to being a change in the DNA that the person is born with) and are called “somatic” mutations.
Subtypes
Under each cancer umbrella, there are actually many different rare diseases. Take breast cancer as an example. By most accounts there are four established subtypes, defined based on how the cancer “looks”, both as you would view it under a microscope and on the molecular level.
For instance, a “HER2+” cancer displays the “Human Epidermal Growth Factor Receptor 2” (HER2) molecule on its surface but doesn’t display the estrogen receptor (ER) or progesterone receptor (PR), molecules that catch certain hormones as they pass by.
Cancers overexpressing HER2 can be treated with specific drugs targeting the HER2 molecule. But if breast cancer is triple negative, meaning it doesn’t display any of these three receptors (HER, ER, or PR), then drugs that target these molecules won’t be effective against the cancer.
Genetics Informed Clinical Trials
The DNA that someone is born with differs in various places from person to person (so-called “germline” variation) and can also impact the course of treatment.
Most clinical trials performed today do not incorporate genetic testing into the trial’s design. When they discover that some trial participants react poorly while others are super responders, they look to data points such as age, other diseases the patient is suffering from, or medications he or she is taking. But the explanation may lie deep down in the DNA — subtle differences in the barcode might be enough for some trial participants to develop an adverse reaction while other people taking the drug derive benefit without harm.
Scientists are now learning more about different cancers by characterizing the mutations driving the tumor and a person’s unique variants that he or she was born with. The course of cancer depends on both the signature of the tumor, something that stems from you but takes on its own life, and you – the host – a necessary participant in the fight against cancer.